1891: Gluck’s Ivory Hip
The first successful hip replacement was pioneered in Germany by Themistocles Gluck, who used ivory to replace the femoral head, securing it in place with nickel plated screws, glue, and plaster of Paris [1].
1950s: McKee-Farrar Metal-on-Metal prosthesis
George Mckee, an English surgeon, was the first to use a cobalt-chrome metal-on-metal prostheses. Initially relatively successful with one recent study showing a 28 year survival rate of 74% [2]. But this method grew unpopular by the mid 1970s due to patient discomfort and increasing implant failure – mainly due to the deleterious effects of metal wear debris and implant dislocation.
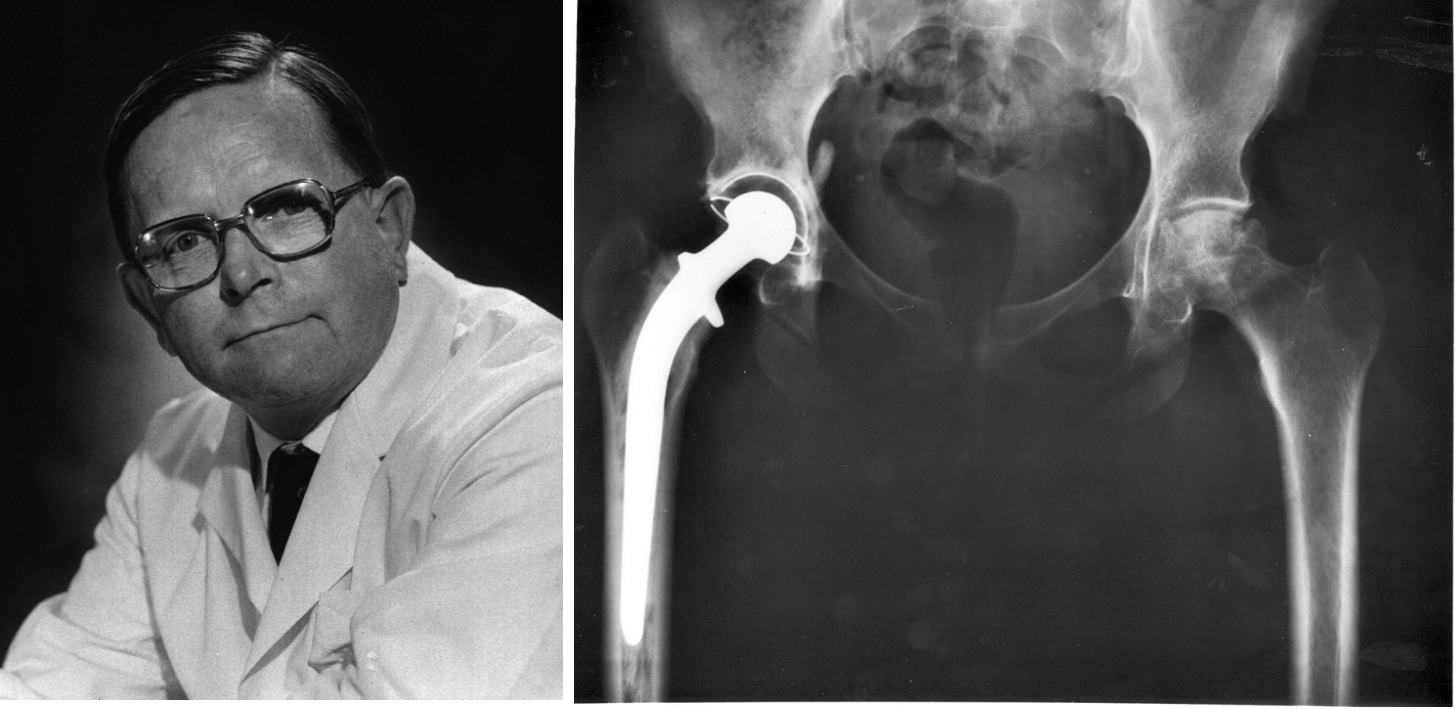
1960s: Sir John Charnley
Following a illustrious career in conservative fracture treatment, in 1961 Charnley (who many still consider the father of hip replacement) developed the first polymer-on-metal hip replacement. In principal, this exact type of hip replacement is still the predominant gold-standard used today comprising of an metal femoral component, a low friction polyethylene acetabular cup, and acrylic bone cement [1, 3].
1970s – 1980s: Developments against wear, metalosis, and osteolysis
Even with the low friction advancement of metal-on-polymer bearing couples, polymeric and metal wear debris still lead to deleterious in vivo reactions leading to pseudotumors and bone resorption which in many cases lead to implant failure and complex revisions.
Following this was a trend of geometry and material advancements including new generations of metal-on-metal (longer lifespan, but released metal ions are highly toxic and carcinogenic) and ceramic-on-ceramic (ultra low wear, though expensive, and can fail catastrophically) bearing couples along with improvements to polymer processing for improved wear resistance [4].
1990s: Second generation hip replacement survivorship plateau
With the popularity of join replacement surgery still steadily increasing it became possible to conduct large qualitative patient surveys to assess hip replacement survivorship, in the 1990s this plateaued to ≤ 90% after 10 years in the patient (depending on the study and replacement hardware) [5]. The success rates of hip replacements are similar even now at ~ 90% – with consistently poorer success in young active patients [6].
2010: DePuy Hip Recall
The challenges of developing materials for high cyclic loading in harsh in vivo environments are immense, but the consequences of messing it up are even bigger.
The ASR XL Acetabular metal-on-metal hip was implanted into 90,000+ patients worldwide. DePuy issued a recall following reports of approximately 1 in 8 replacements failing within 5 years, subsequently leading to lawsuits totaling just under $500 million [7].
High rates of implant failure was due to significant wear leading to release of metal ion debris causing symptoms including chronic inflammation, tissue and nerve damage, and necrosis. Many agree failure was due to a change in geometry and surface treatment of the CoCr alloy that was insufficiently investigated for its tribological performance [8].

2014: Improving simulation and pre-clinical testing
Failure to implement adequate pre-clinical testing leads to poor outcomes including the loss in the quality of life and continued disability for the patient. As a response to this debate LifeLongJoints (LLJ – lifelongjoints.eu), an EU FP7 activity, also led by the co-ordinator of BioTrib, delivered new standards for hip replacements, and a range of new, improved simulators which can provide adverse as well as standard cycles to the implant. These simulators have been commercialised for sale in the UK and abroad by Simulation Solutions, a partner organisation of BioTrib.
2017: Increasing Joint Replacement Needs
Worldwide (for OECD countries) in 2017, 182 and 132 per 100,000 surgeries for hip and knee replacements were performed. These rates continue to trend upwards, for example from 2007 and 2017 overall hip replacement surgeries have increased by 30% and knee replacement by 40% [9]. This translates to an economic figure of between €3B to €5B in implant costs alone [10].
Disconcertingly, the largest increase is in younger, more active patient groups. By 2030 it is projected 52% of hip replacement and 55% of knee replacement recipients will be younger than 65. With current technology, many will wear out these replacements and require complex, costly, and risky revision surgeries [11, 12].
2021+: Future trends in joint replacement
There is a growing trend in increasing implantation accuracy, minimally invasive or more ‘natural’ custom interventions, and improved bearing materials – in many cases materials designed to mimic cartilage and natural anatomy. Current technology pushes are focusing on 3D-printing implants, advanced coatings and soft materials, robotic surgery, tissue and bone preserving implants, and improvements to pre-clinical simulation and testing to assure implant success [1, 13, 14].

BioTrib ETN
The shortage of STEM based researchers within the EU is well recorded [15, 16].
The EU-funded BioTrib program is dedicated to training Early Stage Researchers with the technical and innovation skills to develop advances in the performance of natural and artificial joints. The new program’s focus is on biotribology, which includes friction, lubrication and wear in these interventions. The researchers will gain the highly interdisciplinary skills to shape the next generation of long lasting joint replacement materials and technology.
