Cartilage-related diseases are a promising field to explore in tissue engineering and regenerative medicine. The cartilage hydrated structure is aneural, avascular, and non-lymphatic, which complicates natural regeneration [1,2]. The increase in life expectancy and obesity is directly correlated to osteoarthritis –the disease caused by the degradation of cartilage. The painful consequences also increase comorbidities and burden patients and healthcare providers with exorbitant costs [3,4].
Currently, surgical and non-surgical therapies are employed to address osteoarthritis. They are not permanent solutions [5–7]. Therefore, several groups are developing hydrogels [8,9], electrospun mats [10], and other biomaterials to mimic the natural properties of cartilage. These implants can increase patients’ quality of life, reducing pain, comorbidities, and other undesirable effects after their clinical trials and regulatory agency approval.
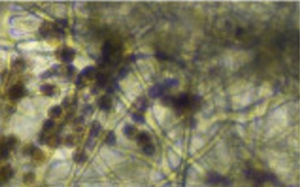
Yilmaz and Zeugolis discuss the promises, challenges, and future perspectives of electrospinning applied to cartilage tissue engineering [11]. They emphasize that although electrospinning literature is abundant in the Pubmed database, few studies explore electrospining’s potential applied to cartilage tissue engineering. The authors demonstrate with pre-clinical results that stem cell-seeded electrospun scaffolds combined with other techniques (3D printing and freeze-drying) can recover lubricating properties, mechanical resistance and restore cartilage tissue properties [11]. Although the reviewed studies consider small animals (rats, mice, and rabbits), they are promising to people suffering from the pain and harmful effects of osteoarthritis worldwide [11].

This article was written by André Plath as part of an ongoing series of scientific communications written and curated by BioTrib’s Early Stage Researchers.
André is researching Boundary Lubrication of Fibrous Scaffolds at ETH Zürich, Switzerland.
.
[1] L.M. Billesberger, K.M. Fisher, Y.J. Qadri, R.L. Boortz-Marx, Procedural Treatments for Knee Osteoarthritis: A Review of Current Injectable Therapies, Pain Res. Manag. 2020 (2020) 1–11. https://doi.org/10.1155/2020/3873098.
[2] E.D. Bonnevie, V.J. Baro, L. Wang, D.L. Burris, Fluid load support during localized indentation of cartilage with a spherical probe, J. Biomech. 45 (2012) 1036–1041. https://doi.org/10.1016/j.jbiomech.2011.12.019.
[3] S. Glyn-Jones, A.J.R. Palmer, R. Agricola, A.J. Price, T.L. Vincent, H. Weinans, A.J. Carr, Osteoarthritis, in: Lancet, Lancet Publishing Group, 2015: pp. 376–387. https://doi.org/10.1016/S0140-6736(14)60802-3.
[4] D.J. Hunter, L. March, M. Chew, Osteoarthritis in 2020 and beyond: a Lancet Commission, Lancet. 396 (2020) 1711–1712. https://doi.org/10.1016/S0140-6736(20)32230-3.
[5] Y. Lee, J. Choi, N.S. Hwang, Regulation of lubricin for functional cartilage tissue regeneration: a review, Biomater. Res. 22 (2018) 9. https://doi.org/10.1186/s40824-018-0118-x.
[6] G. Musumeci, C. Loreto, M.L. Carnazza, F. Coppolino, V. Cardile, R. Leonardi, Lubricin is expressed in chondrocytes derived from osteoarthritic cartilage encapsulated in poly(ethylene glycol) diacrylate scaffold, Eur. J. Histochem. 55 (2011) 31. https://doi.org/10.4081/ejh.2011.e31.
[7] W. Kabir, C. Di Bella, I. Jo, D. Gould, P.F.M. Choong, Human Stem Cell Based Tissue Engineering for In Vivo Cartilage Repair: A Systematic Review, Tissue Eng. Part B Rev. 27 (2021). https://doi.org/10.1089/ten.teb.2020.0155.
[8] Y. Gombert, R. Simič, F. Roncoroni, M. Dübner, T. Geue, N.D. Spencer, Structuring Hydrogel Surfaces for Tribology, Adv. Mater. Interfaces. 6 (2019) 1901320. https://doi.org/10.1002/admi.201901320.
[9] M. Jurak, A.E. Wiącek, A. Ładniak, K. Przykaza, K. Szafran, What affects the biocompatibility of polymers?, Adv. Colloid Interface Sci. 294 (2021) 102451. https://doi.org/10.1016/j.cis.2021.102451.
[10] J.K. Wise, A.L. Yarin, C.M. Megaridis, M. Cho, Chondrogenic Differentiation of Human Mesenchymal Stem Cells on Oriented Nanofibrous Scaffolds: Engineering the Superficial Zone of Articular Cartilage, Tissue Eng. Part A. 15 (2009) 913–921. https://doi.org/10.1089/ten.tea.2008.0109.
[11] E.N. Yilmaz, D.I. Zeugolis, Electrospun Polymers in Cartilage Engineering—State of Play, Front. Bioeng. Biotechnol. 8 (2020). https://doi.org/10.3389/fbioe.2020.00077.
