Header Image: Two-step Matrix Assisted Chondrocyte Implantation
Osteoarthritis is a condition associated with discomfort and significant challenges for the affected individuals. Pain management often involves the utilization of pain-relieving medications that can potentially lead to dependency [1]. Joint function restoration is achieved through the implementation of metal implants, although their durability is limited. Consequently, a secondary surgical procedure might be necessary as the patient ages. The use of these implants also presents additional complications such as inflammation induced by the gradual wear of microscopic components [2].
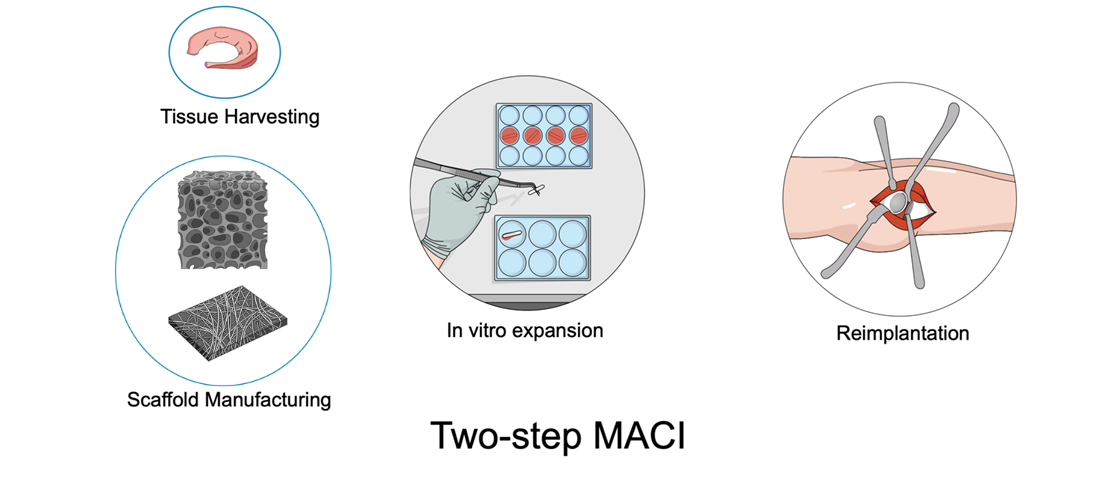
In response to these issues, chondrocyte implantation was introduced during the 1980s in Sweden. This medical procedure involves the extraction of cartilage or stem cells from the patient, which are then propagated within a supportive scaffold material (matrix) [3]. Subsequently, these multiplied cells are reintroduced into the patient’s body (Figure), contributing to tissue regeneration (two steps). An alternative method involves microfracture and scaffold implantation in one step, allowing cells to populate the material and facilitate cartilage reconstruction [3]. These newer techniques exhibit improved rates of success when compared to external cartilage growth [4].
However, a key challenge emerges when cartilage cells transform, losing their original properties. As a result, the newly generated tissue tends to become less lubricant. This phenomenon arises due to the limitations of the scaffold in replicating the intricate conditions found within living tissue [5]. The implications of this could involve detachment or accelerated wear of the implant, necessitating further surgical intervention, and potentially even the use of metal implants. Current materials utilized include foam structures derived from pork collagen or laser-etched plastics [6,7]. Nonetheless, promising advancements are being explored in the experimental phase, involving bio-based materials produced through techniques like 3D printing and fiber integration. One notable application of these innovations is the potential to postpone the need for a prosthesis, thereby offering a beneficial outcome, particularly for younger patients.
References
[1] L.M. Billesberger, K.M. Fisher, Y.J. Qadri, R.L. Boortz-Marx, Procedural Treatments for Knee Osteoarthritis: A Review of Current Injectable Therapies, Pain Res. Manag. 2020 (2020) 1–11. https://doi.org/10.1155/2020/3873098.
[2] O. Hussain, B. Ahmad, S. Saleem, Biomaterials for Artificial Knee Joint Replacement: A Review, Int. J. Mater. Eng. Innov. 14 (2023) 1. https://doi.org/10.1504/IJMATEI.2023.10048812.
[3] G. Filardo, E. Kon, A. Roffi, A. Di Martino, M. Marcacci, Scaffold-Based Repair for Cartilage Healing: A Systematic Review and Technical Note, Arthrosc. J. Arthrosc. Relat. Surg. 29 (2013) 174–186. https://doi.org/10.1016/j.arthro.2012.05.891.
[4] M.R. Steinwachs, J. Gille, M. Volz, S. Anders, R. Jakob, L. De Girolamo, P. Volpi, A. Schiavone-Panni, S. Scheffler, E. Reiss, U. Wittmann, Systematic Review and Meta-Analysis of the Clinical Evidence on the Use of Autologous Matrix-Induced Chondrogenesis in the Knee, CARTILAGE. 13 (2021) 42S-56S. https://doi.org/10.1177/1947603519870846.
[5] A.R. Armiento, M.J. Stoddart, M. Alini, D. Eglin, Biomaterials for articular cartilage tissue engineering: Learning from biology, Acta Biomater. 65 (2018) 1–20. https://doi.org/10.1016/j.actbio.2017.11.021.
[6] J.L. Carey, A.E. Remmers, D.C. Flanigan, Use of MACI (Autologous Cultured Chondrocytes on Porcine Collagen Membrane) in the United States: Preliminary Experience, Orthop. J. Sports Med. 8 (2020) 232596712094181. https://doi.org/10.1177/2325967120941816.
[7] V.M. Mehta, S. Mehta, S. Santoro, R. Shriver, C. Mandala, C. Weess, Short term clinical outcomes of a Prochondrix® thin laser-etched osteochondral allograft for the treatment of articular cartilage defects in the knee, J. Orthop. Surg. 30 (2022) 102255362211417. https://doi.org/10.1177/10225536221141781.

This article was written by André Plath and Giulio Cavaliere as part of a series articles curated by BioTrib’s Early Stage Researchers.
André is one of BioTrib’s Early Stage Researcher‘s who is investigating Boundary Lubrication of Fibrous Scaffolds at ETH Zürich, Switzerland.