Back in 2013, I used to volunteer for a community-based non-profit organisation that provides HIV/AIDS education, prevention, care, and support programmes in conservative Malaysia. Their main office is located on a first floor of shop lot in the seedy part of Kuala Lumpur. Every time I walked up the stairs, I would be greeted by a poster that says ‘Discrimination kills, not AIDS’ which has faded over the years. It was a reminder for all to leave their prejudice behind upon entering. For 2 hours, twice a week, I would carry out an anonymous rapid HIV antibody test for marginalised community of Kuala Lumpur and providing counselling and education on sexuality and sex-related issues in a non-judgemental way.
Millions have died from Covid-19 but it is only the second highest death tolls of global infectious disease pandemic in the last century after HIV/AIDS. Progress in eradicating HIV/AIDS has been painfully slow despite almost reaching its 4th decade and millions more death since it was first discovered. Covid-19 pandemic has proved that lives can be saved from expedited, concerted effort from everyone in record time. This raises the question of whether HIV/AIDS patients’ demographic was the main reason for the lack of appetite to fund or eradicating this problem?
The current daily anti-retroviral treatment for HIV has helped people to have near-normal life expectancy as well as managing it like a chronic condition rather than a death sentence. In 2021, another breakthrough for HIV when long-acting ART injection was approved by NICE [1]. This treatment will reduce the burden of daily dosage to once every 2 months which will improve patients’ compliance and managing the problem better. To give sense of the timeline, the daily combined ART was first introduced in 1995, more than a decade ago [2]. The NHS also has been offering free Pre-exposure Prophylaxis (PrEP) since 2020 for HIV negative who are at risk of being exposed to the virus. This decision was taken after an overwhelming positive outcome from IMPACT trials which was consistently oversubscribed from those who are interested to take part and had to be on waiting list for months. The same affirmative outcome has been seen in other trials all over the globe [3].
Currently, only men who have sex with men AND who have had the same sexual partner for 3 months or more are able to give blood in the NHS. These criteria were only being introduced in Summer 2021 after a lengthy campaign for risk-based assessment for blood donation amongst gays. Ten years before that, a total ban was in place for all men who have sex with another men. Earlier this month, Terrence Higgin Trust reported that new HIV diagnoses amongst heterosexual people have overtaken from those in gay and bisexual men in 2020 [4]. If we are ‘following the science’, shouldn’t the risk-based assessment for blood donor applicable for everyone who wanted to donate blood, given the new data presented and not just our preconceived idea of it is a ‘gay disease’?
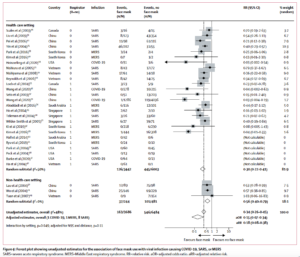
Covid-19 also has brought up some of the prejudice that have been lurking in the subconscious mind of science. The advice on the use of face coverings was only introduce by the UK Government and WHO in June 2020 citing there was ‘lack of scientific evidence’ prior to that. A meta-analysis study on usage of face masks during infectious disease pandemics funded by WHO that was published in The Lancet [5] has since changed their stance. Looking back at the scientific paper, out of 23 studies on face masks, only 3 were conducted during 2020 Covid-19 pandemic. 20 other studies were conducted during SARS or MERS outbreaks, a dozen of them has been published for more than a decade before, where majority of them were in East Asia. Only 3 studies were in a non-healthcare setting. Was it really ‘lack of evidence’ or our prejudiced has blinded us again towards the good public health practice from nations that have a different ethnicity culture or who are not aligned with our belief? Were we right to “err on the side of caution” towards South Africa when Omicron variant was first detected?
Discrimination and prejudice have been the fabric of humanity since the beginning of time. As a human being, we all need to proactively be kind towards each other regardless of your moral values. As a scientist, we must not let our biases eclipse our scientific rigour. There should not be a place for prejudice in science, or anywhere for that matter. That 90’s poster might have been faded, but the message still rings truth to this day. For LGBT+ History Month, let us remember that our work in ending discrimination will NEVER end. The work will always require an active participation and effort from everybody – scientists are no exception.
This article was written by Faizal Kamarol Zaman as part of a series on LGBTQ+ History Month and prejudice in STEM.
References
[1] https://www.bbc.co.uk/news/health-59330979
[2] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4309625/
[3] https://www.iwantprepnow.co.uk/prep-trials/
[4] https://www.tht.org.uk/news/heterosexual-hiv-diagnoses-overtake-those-gay-men-first-time-decade
[5] https://www.sciencedirect.com/science/article/pii/S0140673620311429